Policy
The NCDI Poverty Network supports health leaders as they develop policies that prioritize equitable, cost-effective health interventions.
National NCDI Poverty Commissions—which are composed of Ministry of Health policymakers, clinicians, academic researchers, health planning and financing experts, implementing partners and donors, and people living with severe conditions—are the backbone of the NCDI Poverty Network.
The Network’s Policy Team works with National Commissions to develop policies that prioritize equitable, cost-effective interventions to address severe conditions disproportionately affecting children and young adults living in extreme poverty. In particular, the Policy Team supports National Commissions in countries that have recently joined the Network in working through the first phase of the Network’s Four-Phase Theory of Change: Situation Analysis and Priority-Setting.
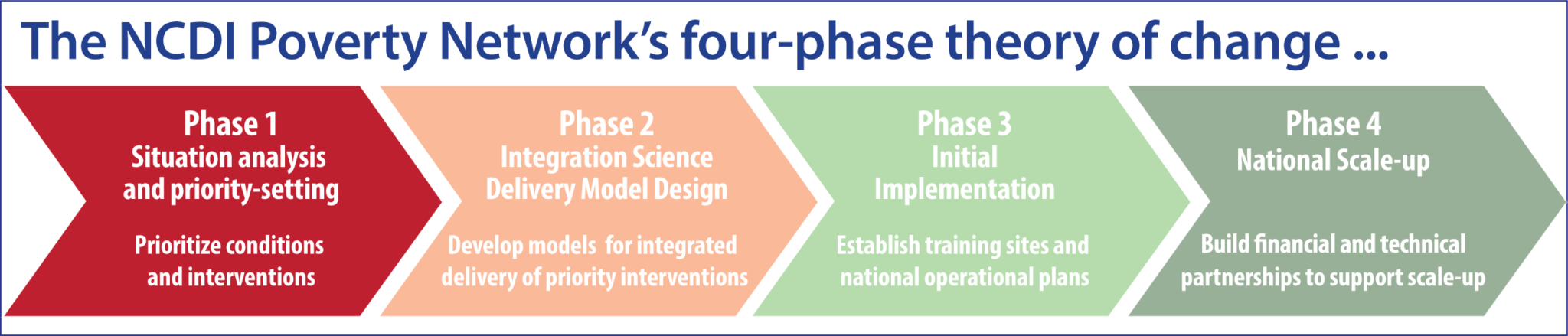
During this first phase of the Network process, National Commissions analyze the national burden of NCDs and injuries, disaggregated by age, sex, and socioeconomic status, and assess the availability and coverage of NCDI services at different levels of the health system, in order to understand disparities in prevalence, access to services, and outcomes for poor and marginalized populations. Based on findings from this situation analysis, Commissions then prioritize conditions and interventions to address the burden, taking into account both cost-effectiveness and equity, and estimate the cost and potential impact of prioritized interventions as well as the fiscal space required to implement them. Finally, Commission members disseminate their key findings and recommendations to elevate equitable access to care and treatment for severe conditions that disproportionately impact the poorest children and young adults as a priority for national policies and financing.
The Policy Team supports countries through this process by:
Sharing analytical frameworks, methods, and tools developed by the Lancet NCDI Poverty Commission, as well as a priority-setting tool developed in collaboration with the Center for Integration Science in Global Health Equity research team and the Bergen Center for Ethics in Priority-Setting;
Facilitating exchanges of experience and lessons learned with more than a dozen countries that have successfully completed this phase; and
Assisting with preparation and dissemination of reports summarizing their key findings and recommendations.
Policy and National Commission Updates
The Kenya Ministry of Health, NCD Alliance Kenya, NCDI Poverty Network, and partners convened for Kenya’s inaugural National NCD Conference, which featured the launch of a PEN-Plus National Operational Plan.
The October tour showed the strong work of a relatively young PEN-Plus program that is poised for growth, reflecting the adaptability of the integrated model of care for noncommunicable diseases.
The same week that global policy talks on noncommunicable diseases were taking place at the United Nations General Assembly in New York City, health leaders in Abuja, Nigeria, were marking progress in being able to provide care for people living with severe, chronic NCDs through PEN-Plus.
Zambia health officials recently opened the country’s fourth and fifth PEN-Plus clinics, marking both occasions within weeks of launching the country’s national operating plan for the care of people living with severe noncommunicable diseases. Both new clinics have received support from the Scottish Government.
In a launch event in late July, the Republic of Somaliland announced a partnership with the NCDI Poverty Network to support people living with severe, chronic noncommunicable diseases through PEN-Plus. In a statement, the Ministry of Health Development of the Republic of Somaliland noted the partnership “marks a significant step forward in strengthening the ministry’s efforts to improve health services, particularly in addressing noncommunicable diseases.”
The second International Conference on PEN-Plus in Africa positioned Nigeria as a leading advocate for PEN-Plus across the African continent, media coverage of the July conference showed.
Zambia health officials recently took a significant step forward in PEN-Plus implementation with the launch of a national operational plan to support and expand care for people living with severe, chronic noncommunicable diseases. The Centre for Infectious Disease Research in Zambia, or CIDRZ, a PEN-Plus implementing partner working with the NCDI Poverty Network, hosted a launch event in Lusaka.
Dr. Ana Mocumbi, co-chair of the NCDI Poverty Network, recently received the Republic of Mozambique’s Medal of Merit for Science and Technology. The honor recognizes her outstanding contributions to science, technology, and innovation in Mozambique.
Health officials from several French-speaking countries in western and central Africa have begun meeting in a new webinar series to share—in French—their challenges and successes in expanding care for people living with severe noncommunicable diseases. The new series solidifies a groundbreaking collaboration that began with a February study tour in Sierra Leone.
On behalf of the NCDI Poverty Network, Rachel Gasana, senior director of advancement, testified at the multistakeholder hearing on noncommunicable diseases, held at the United Nations Headquarters in New York City. The Network was one of 70 organizations selected to deliver testimonies as a prelude to the United Nations High-Level Meeting on NCDs in September.
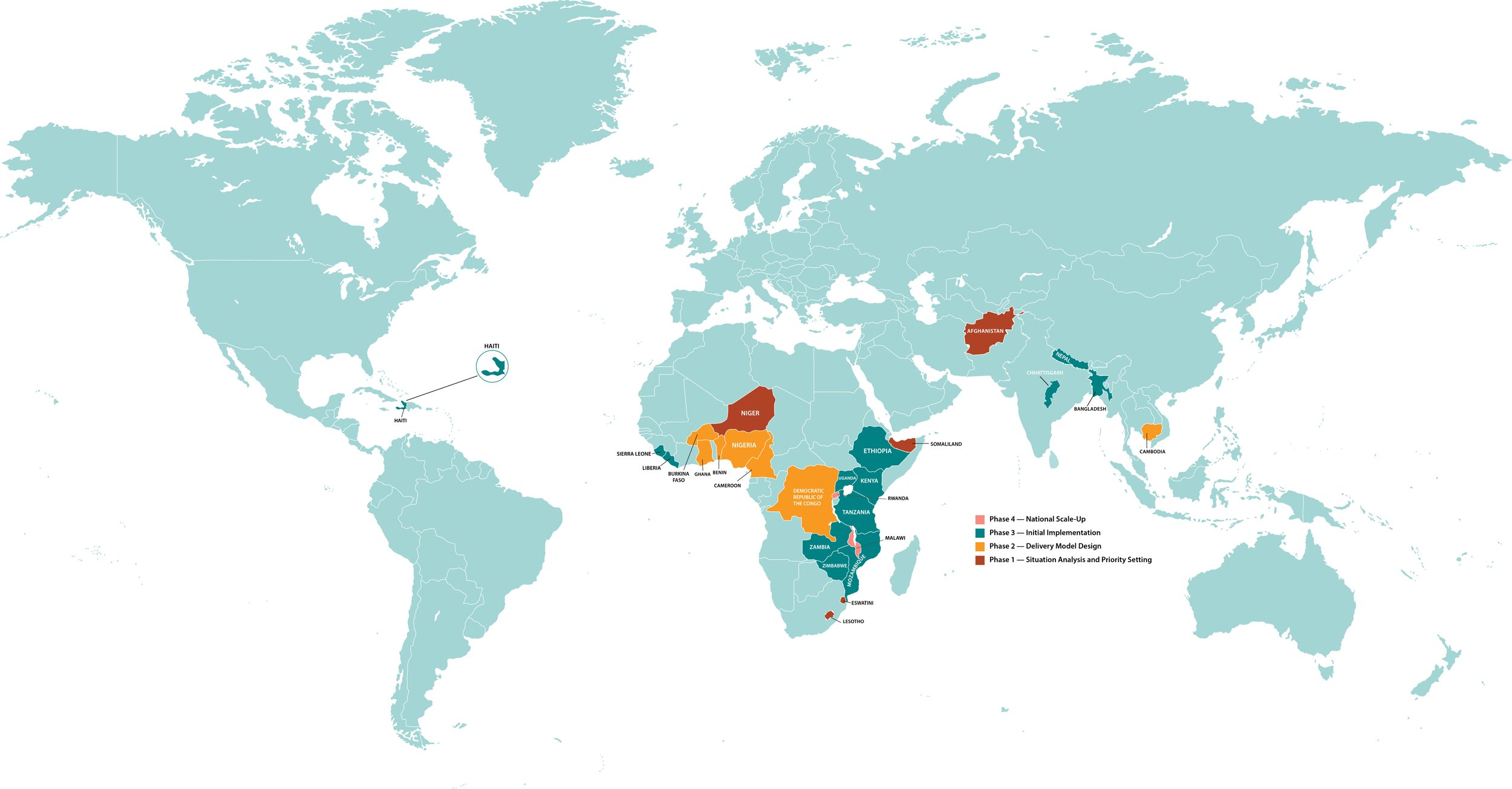
In just the past several months, the NCDI Poverty Network has grown from 23 partner countries to 27, with the most recent additions being Eswatini, Lesotho, Niger, and Somaliland.
An audience of patients, clinicians, Ministry of Health officials, and community members recently gathered to celebrate a historic milestone for Sierra Leone: the launch of a purpose-built PEN-Plus clinic at Koidu Government Hospital. Partners In Health, the implementing partner for PEN-Plus in Koidu, has published an account of the clinic’s services.
Zimbabwe recently finalized its national operational plan for PEN-Plus, becoming the first country to do so among the dozen nations that began implementing PEN-Plus in 2022–23. “This plan shows the great commitment of Zimbabwe’s Ministry of Health and its supporting partners to take the lessons learned from its initial experience with PEN-Plus to the next level,” said Dr. Neil Gupta, senior director of policy for the NCDI Poverty Network.
The NCDI Poverty Network has submitted proposals to the World Health Organization suggesting it add analogue insulins and a triple fixed-dose antihypertensive medicine combination to its Model List of Essential Medicines. The Network has also proposed that WHO reclassify hemoglobinopathies to shine more of a spotlight on sickle cell disease and thalassemias.
The WHO Regional Office for Africa recently published a landmark report that details the impact and momentum of the PEN-Plus model, providing a valuable tool for advocacy and information about integrated care for people living with severe, chronic noncommunicable diseases.
Dr. Neil Gupta, a pediatrician and the senior director of policy at the NCDI Poverty Network, will join a panel of healthcare providers in an upcoming webinar that explores how PEN-Plus affects the care of children living with severe NCDs. The International Pediatric Association is hosting the webinar on March 25.
The NCDI Poverty Network’s recent week of advocacy in Rwanda included visits to two hospitals, a conference with more than 700 attendees, a panel with four expert speakers, and one recurring theme: the recognition that PEN-Plus is an effective model for mobilizing action and financing to increase access to care for people living with severe, chronic noncommunicable diseases.
A “game-changing” study tour of a PEN-Plus clinic in Sierra Leone introduced Ministry of Health officials from six other Francophone nations to the role integration can play in providing quality care for people living with severe noncommunicable diseases in low- and lower-middle-income countries.
The NCDI Poverty Network—through one of its co-secretariats, the Center for Integration Science in Global Health Equity at Brigham and Women’s Hospital—has joined UNICEF in publishing a report on the burden on noncommunicable diseases on children, adolescents, and young adults in South Asia.
After several years of hard work, members of the Nigeria NCDI Poverty Commission have published their final Phase 1 report.
On September 24, the Network officially published the PEN-Plus Partnership Strategic Plan (2025–2028). “It is our commitment, our testimony, and our witness to the collective progress of NCDI Poverty Network partners in delivering healthcare and hope to people in lower-income countries,” said Dr. Gene Bukhman, co-chair of the Network.
The NCDI Poverty Commission of the Democratic Republic of the Congo has published its final Phase 1 report.
In early June, delegations from all eight countries in UNICEF ROSA—the Regional Office for South Asia—convened in Kathmandu for a three-day workshop on severe childhood-onset noncommunicable diseases.
In early June, delegations from all eight countries in UNICEF ROSA—the Regional Office for South Asia—convened in Kathmandu for a three-day workshop on severe childhood-onset noncommunicable diseases.
In recognition of World Sickle Cell Day on June 19, a Lancet Haematology editorial cited both PEN-Plus and the first International Conference on PEN-Plus in Africa as initiatives that can help ensure improved access to diagnosis, treatment, and care for people living with sickle cell disease in low- and middle-income countries.