Type 1 Diabetes
PEN-Plus for People Living with Type 1 Diabetes
Unlike their counterparts in high-income countries, children with type 1 diabetes in rural areas of sub-Saharan Africa often die within a year of diagnosis. This tragedy is as medically unnecessary as it is unjust.
To address inequities in care, the NCDI Poverty Network is working with 22 resource-poor countries around the world to implement PEN-Plus, an innovative, integrated-care delivery model for severe, chronic noncommunicable diseases such as type 1 diabetes, sickle cell disease, and childhood heart diseases. PEN-Plus clinics save the lives of those with type 1 diabetes, for example, by providing insulin and specialized care close to home, as well as money for food and transportation to the clinic.

“That night, my blood pressure got so high I started talking nonsense and passed out. My parents were terrified and took me to the health center. I was in a coma for five days before regaining consciousness. Symaque [a PEN-Plus nurse] taught me how to inject myself, so I could take my insulin to school with me.”
—Angelique Mukarakisa, a young woman living with type 1 diabetes in rural Rwanda
Meet People Living with Type 1 Diabetes in PEN-Plus Countries
Type 1 Diabetes Updates
With peer support having proved to be a key component of PEN-Plus care, the NCDI Poverty Network is developing an integrated training program for peer educators. “We’ve seen beautiful examples of young people who are unafraid to speak boldly about their condition, to be advocates, to be champions,” said Dr. Colin Pfaff, the Network’s associate director of programs. “They are living successful lives and are examples to others, which has such a powerful impact.”
A recently published study found that patient education and peer support helped people living with type 1 diabetes in rural Liberia manage their disease. “Their extra barriers to health,” said Dr. Alma Adler, the Network’s research director, “make it even more critical for patients in low-resource settings to gain both problem-solving skills and a strong clinical understanding of their condition.”
For several years, without funds for transportation or food, Yismaw Nigussie, a 15-year-old living in rural northern Ethiopia, would risk his health even getting to the clinic that provided treatment for his type 1 diabetes. Then a routine assessment changed the trajectory of his life.
The PEN-Plus model of care is not only improving treatment and accessibility for people living with type 1 diabetes, but it’s also placing an emphasis on the disease that had not previously existed in some parts of the world, Dr. Gene Bukhman said during the recent International Society for Pediatric and Adolescent Diabetes conference, held in Montreal.
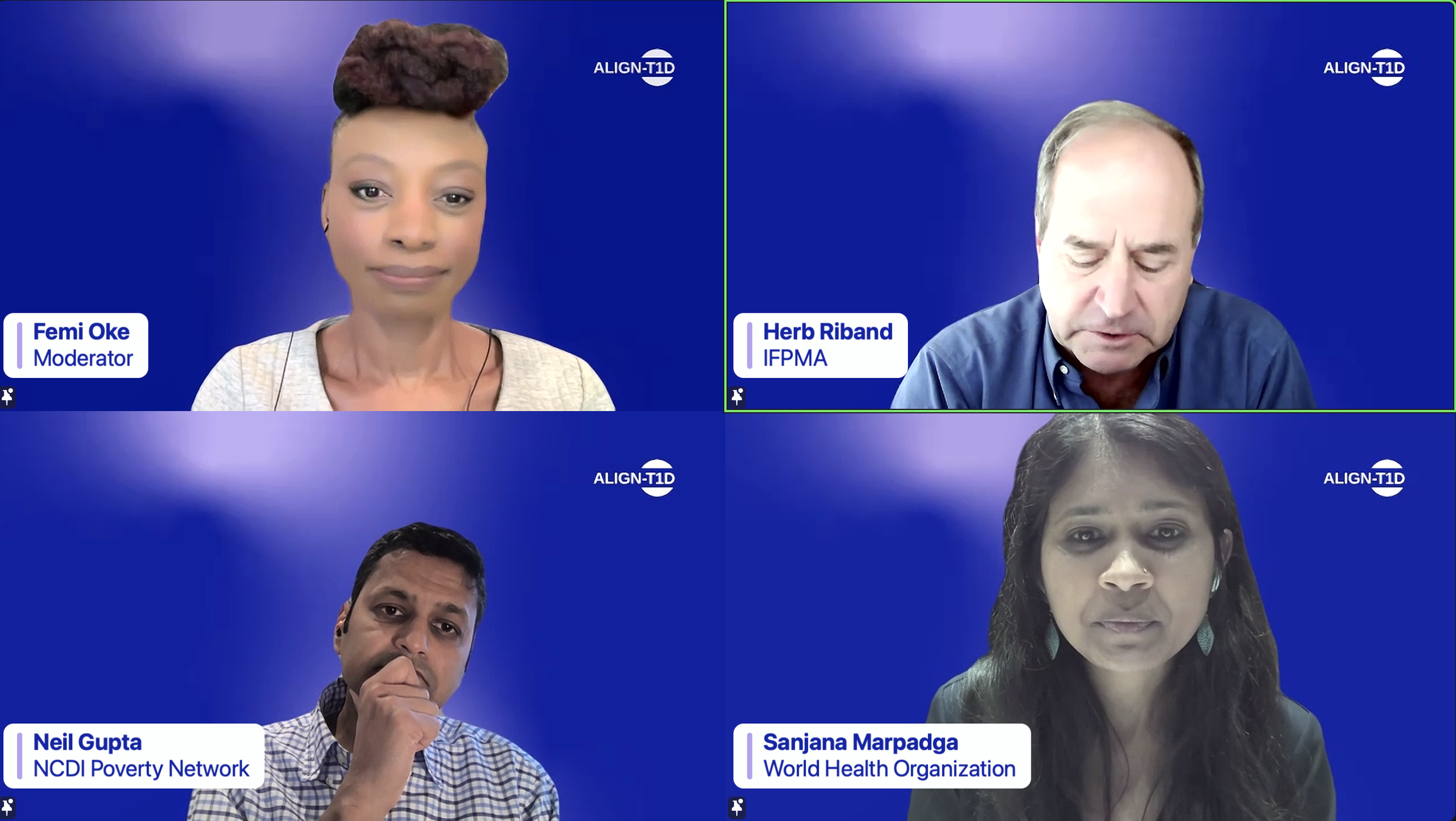
ALIGN-T1D includes global funders of type 1 diabetes programs, leading producers of diabetes medicines and technologies, and members of the worldwide type 1 diabetes community.
Naomi Mwila was attending college for civil engineering, planning her career, and dreaming of a bright future until a diagnosis of type 1 diabetes changed her entire outlook, as a college professor told her that her condition meant she no longer had anything to live for. Then an integrated PEN-Plus camp restored her ability to dream.
When it comes to advocating for health equity and greater access to care for people living with severe noncommunicable diseases, Emmanuella Selasi Hormenoo doesn’t miss an opportunity. Undaunted by sharing stages with global health leaders, the Voices for PEN-Plus advocate represented people with lived experience on two panels at the World Health Summit in Berlin in mid-October.
Camp Tuli Bonse, an integrated summer camp, will bring together about 60 children, adolescents, and young adults living with either type 1 diabetes or sickle cell disease for a week of health education, support, solidarity, and fun in Chongwe, Zambia, from August 18 to 22.
The second International Conference on PEN-Plus in Africa (ICPPA 2025) will convene on July 8–10 in Abuja, Nigeria, with virtual participation available to healthcare professionals, researchers, and policymakers worldwide.
The NCDI Poverty Network has submitted proposals to the World Health Organization suggesting it add analogue insulins and a triple fixed-dose antihypertensive medicine combination to its Model List of Essential Medicines. The Network has also proposed that WHO reclassify hemoglobinopathies to shine more of a spotlight on sickle cell disease and thalassemias.
The NCDI Poverty Network’s recent week of advocacy in Rwanda included visits to two hospitals, a conference with more than 700 attendees, a panel with four expert speakers, and one recurring theme: the recognition that PEN-Plus is an effective model for mobilizing action and financing to increase access to care for people living with severe, chronic noncommunicable diseases.
As a panelist during a recent international diabetes conference in Copenhagen. Dr. Ana Mocumbi, co-chair of the NCDI Poverty Network, highlighted the power of integration in helping to achieve global health equity.
The NCDI Poverty Network—through one of its co-secretariats, the Center for Integration Science in Global Health Equity at Brigham and Women’s Hospital—has joined UNICEF in publishing a report on the burden on noncommunicable diseases on children, adolescents, and young adults in South Asia.
In a new video, Lucy Johnbosco, a member of the NCDI Poverty Network’s Steering Committee from Tanzania, offers her perspective of what it takes to change perceptions of type 1 diabetes in places where many people have limited understanding of the condition.
Two NCDI Poverty Network physicians lent their expertise during a recent diabetes training workshop that the Sonia Nabeta Foundation hosted in Uganda.
The NCDI Poverty Network has published a French edition of PEN-Plus Clinical Tools and Programmatic Standards, a document that defines the diagnostic, treatment, and patient support services that compose PEN-Plus. Several francophone countries have already initiated PEN-Plus.
Camps that bring together young people living with a severe noncommunicable disease are showing that the benefits of integrated care can extend far beyond clinical settings. The first such camps—held this year in Rwanda and Zimbabwe—hosted young people with type 1 diabetes, sickle cell disease, and childhood heart disease.
In recognition of World Diabetes Day, educator and advocate Edith Mukantwari shares her personal story of living with type 1 diabetes in Uganda, the lessons she’s learned, and the importance of a supportive community.
The International Society for Pediatric and Adolescent Diabetes meeting in October shined a spotlight on patient advocates as key stakeholders in developing guidelines for type 1 diabetes care globally.
The PEN-Plus Partnership Strategic Plan (2025–2028) had its official launch at Springboard for Action, an event celebrating progress toward global access to care for people living with severe, chronic noncommunicable diseases. The NCDI Poverty Network hosted the event in New York City in September on the sidelines of the 79th Session of the U.N. General Assembly.
In Springboard for Action, a PEN-Plus celebration held in September on the sidelines of the 79th Session of the U.N. General Assembly, leaders from the World Health Organization’s Regional Office for Africa, UNICEF, and Nigeria’s Ministry of Health and Social Welfare all expressed their commitment to PEN-Plus. The event also featured a performance by the Broadway cast of Disney’s The Lion King.
In August, CIDRZ held a four-day boot camp for young people living with type 1 diabetes in Zambia. The camp combined entertainment and sports activities with education on self-management of the condition.
The Network has published PEN-Plus Clinical Tools and Programmatic Standards, a document aimed at informing clinic planning, budgeting, and operations by providing a crisp definition of PEN-Plus clinical care, including the diagnostic, treatment, and patient support services available.
In recognition of World Sickle Cell Day on June 19, a Lancet Haematology editorial cited both PEN-Plus and the first International Conference on PEN-Plus in Africa as initiatives that can help ensure improved access to diagnosis, treatment, and care for people living with sickle cell disease in low- and middle-income countries.
A recently published study of people living with type 1 diabetes in two rural clinics in Malawi found a high level of acceptability and satisfaction among those using continuous glucose monitoring, suggesting that the technology is feasible in low-income settings.
Following the International Conference on PEN-Plus in Africa, the NCDI Poverty Network hosted the first Voices for PEN-Plus Advocacy Summit. The event, held in Dar es Salaam, Tanzania, on April 26, brought stakeholders together to brainstorm ideas for increasing the scope and effectiveness of advocacy initiatives.
In advance of the International Conference on PEN-Plus in Africa, the NCDI Poverty Network team compiled research resources on PEN-Plus and other integrated-science healthcare delivery models.
“It is inconceivable that a 20-year-old man would weigh only 55 pounds,” said Bright Mailosi, a specialist in noncommunicable diseases. “So much could have been done to intervene when he was first diagnosed with type 1 diabetes. Although I wish PEN-Plus had arrived in Karonga years earlier, I’m excited that we’ve changed the narrative of how complex NCDs are managed in rural areas.”
“Tawonashe is exactly the kind of patient for whom PEN-Plus was designed,” said Dr. Alvern Mutengerere, project manager for noncommunicable diseases at SolidarMed, the implementing partner for the PEN-Plus clinic in Masvingo.
The NCDI Poverty Network has produced “Language Matters,” a primer intended to sensitize PEN-Plus providers to the communication nuances involved in caring for people living with severe, chronic noncommunicable diseases.